Federal regulations set the standards for the effective date of coverage if enrollment is due to a qualifying event.
Carriers can (and some do) make coverage effective sooner than required by the federal standards.
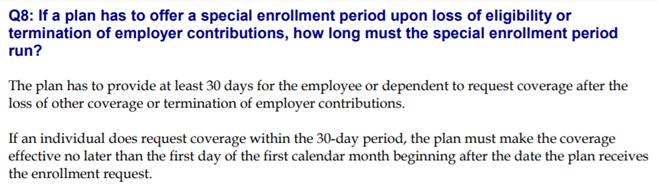
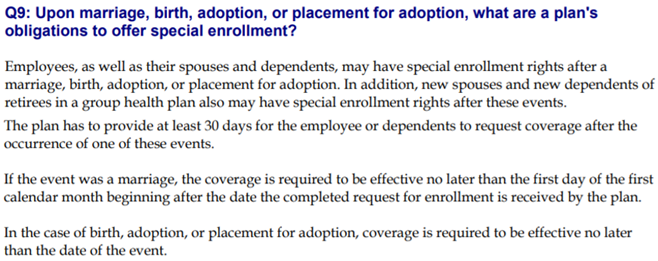
From the Department of Labor’s FAQ document on HIPAA special enrollment rights: https://www.dol.gov/sites/default/files/ebsa/about-ebsa/our-activities/resource-center/faqs/hipaa-compliance.pdf